Introduction
It is estimated that 77 million persons was with diabetes in India in 2020 and in future every fifth person with diabetes will be an Indian. Due to these sheer numbers, the economic burden due to diabetes in India is amongst the highest in the world. The real burden of the disease is however due to its associated complications which lead to increased morbidity and mortality.
Rapid urbanisation and industrialisation have produced advancement on the social and economic front in developing countries such as India which have resulted in dramatic lifestyle changes leading to lifestyle related diseases. The transition from a traditional to modern lifestyle, consumption of diets rich in fat and calories combined with a high level of mental stress has compounded the problem further. The so called “Asian Indian Phenotype” refers to certain unique clinical and biochemical abnormalities in Indians which include increased insulin resistance, greater abdominal adiposity i.e., higher waist circumference despite lower body mass index, lower adiponectin and higher high sensitive C-reactive protein levels. This phenotype makes Asian Indians more prone to diabetes and premature coronary artery disease. At least a part of this is due to genetic factors. The changing life style, lack of exercise, fast foods, sedentary habits, stress and tension are major reasons for causing fresh disease and aggravating an existing condition. So the essential need of today's era is to provide welcoming effects to improve the overall health status of diabetic patient.
Materials and Methods
For the present study 30 patients were selected from inpatient and outpatient department of Panchakarma, National institute of Ayurveda, Jaipur, Rajasthana.
Objective
To evaluate the effect of Panchatikta Pancha Prashritika(PPP) Basti Karma in the management of Madhumeha (Type 2 DM).
Inclusion criteria
Patient of NIDDM with blood sugar level; FBS- 126 to 300 mg/dl or PPBS-180 to 400 mg/dl.
Patient having classical signs and symptoms of the Madhumeha (Diabetes) according to Ayurveda as well as modern medicine.
Age group of 20-60 years.
Patient otherwise healthy and fit for Basti Karma as per the Ayurvedic classics.
Exclusion criteria
Age < 20 yrs and > 60 yrs.
Patients of Madhumeha (Diabetes) having disease chronicity of more than 20 yrs.
Patients of Type-1 Diabetes or the patients of Type-2 Diabetes taking Insulin.
Patients having serious complications of Diabetes like Nephropathy, Neuropathy, Retinopathy, Diabetic Foot, Carbuncles etc.
Patients having drug or chemical induced Type II Diabetes, like glucocorticoids induced or thyroid hormone induced etc.
Diabetes associated with Carcinoma or any other disease affecting multiple body systems.
Pregnancy.
Panchatikta Pancha Prashritika Basti(PPP Basti) Karma
30 Patients of Non Insulin Dependent Diabetes Mellitus were registered. All the patients were examined for general condition and for sign and symptoms of Madhumeha(Diabetes mellitus) and the patients were treated by PPP Basti Karma.
Panch tikta panch prashritika Basti is specifically indicated for the treatment of Madhumeha Hence this Basti was administered in Kala Basti schedule which consist of total 16 number of Basti out of which 6 were Niruha Basti and 10 were Anuvasana Basti.2 As shown in the Table 2.
Preparation of Panchtikta Panch Prashritika Basti:1
Pancha Tikta Pancha Prashritika Basti contain following ingredients in different proportion as shown below:
Raw material for Kashaya (decoction):
Patol patra (Trichosanthes dioica leaf)
Nimba twak (Azadirachta indica bark)
Kiratatikta (Swertia chirata whole plant)
Rasna (Pluchea lanceolata leaf)
Saptaparna (Alstonia scholaris bark)
Honey and rock salt were mixed together in the beginning followed by addition of warm ghee and thoroughly triturated. The finely wet grinded paste of Sarshapa was then added; lastly decoction was added to it. The mixture was then again triturated thoroughly. Mixture is than filtered through sieve and made warm indirectly in water bath. The filtrate so obtained was used as Basti dravya.
Anuvasana Basti
Triphala Siddha Tila taila 60 ml mixed with one gram each of Shatpushpa and Saindhava Lavana was used for Anuvasana Basti after meal.
The required quantity of Triphala Taila indirectly made lukewarm Shatapuspa Choorna and Saindhava Lavana were added then mixed well and again made into lukewarm.
Retension time Yoga-ayoga and Atiyoga of Niruha and Anuvashana Basti are presented in Table 3, Table 4, Table 5, Table 6.
Table 1
Showing kala Basti schedule
Table 2
Average retention time of Anuvasana Basti found in 30 patients of Madhumeha
|
<6 hrs |
6 To 12 hrs |
>12 hrs |
|||
|
No. of Patients |
% |
No. of Patients |
% |
No. of Patients |
% |
|
19 |
63.33 |
11 |
36.67 |
0 |
0 |
Age
In the present study 44.44% patient were between 51- 60 years of age group followed by 27.78% was of 31-40 years and 22.22% was of 41-50 years. This reveals that maximum prevalence of the disease is at Madhyama Vaya. These findings were concordant to the recent statistical data which shows that the onset of Type II Diabetes mellitus after the forties is most common but obese population may get it at an earlier age.
Religion
In this study 73.33% of the patients were Hindu and 25.56% were Muslims with 1.11% of Sikh which indicative of Hindu dominant population of this region.
Marital status
In this study 98.89% patients were married As such, there is no correlation between marital status of patient and Diabetes. As the inclusion criteria for age in this study was between 30–60 years and most of the population in India gets married by 30 years of age, thereby, the maximum number of patients were married.
Occupation
The incidence was more in house wives (33.33%) followed by business person (28.89%). These figures show that disease occurs in those classes who usually lead sedentary life style and eat more than their requirement.
Family history of madhumeha
Around 36.67% of patients had family history of Madhumeha, which reflects the fact that genetic predisposition is strongly associated with the disease. Whereas 63.33% of them did not have positive family history of DM, which certainly gives a hint that the development of Madhumeha is not totally hereditary dietetic and other life style factors plays an important role in the causation of DM.
Agni
Majority of the patients were having Vishamagni (66.67%) followed by Teekshnagni (22.22%) These finding indicates the dominancy of Vata Dosha in the Samprapti of Madhumeha.
Koshtha
Regarding the nature of Koshtha in maximum number of patients, Madhyama Koshtha was noted in 65.56% followed by Krura Koshtha (31.11%) and Mrudu (3.33%). This indicates towards the involvement of Kapha Dosha and Vata Dosha in the pathogenesis of Madhumeha.
Prakruti
Vata Pitta and Pitta Kapha prakriti were predominant in 27.78% and 26.67% of individuals respectively where as Kapha in 17.78%, Kapha Vata and Vata Prakriti in 3.33% each. TriDosha Prakriti in 5.56% of individuals and Pitta Prakruti in 1.11% of patients. This shows that Dvandaja Prakriti persons are more prone for Madhumeha and this may be the reason that Dvandaja Prakriti is considered as Nindya
Abhyavarana shakti
The Abhyavarana Shakti of majority of individuals (74.44%) was Madhyama followed by Pravara (16.64%) and Avara (8.89%). As Kshudhaadhikyata was commonly observed in patients of DM which was also seen in this study.
Jarana shakti
The Jarana Shakti of majority of individuals was Madhyama (34.44%) Followed by Avara (55.56%) and Pravara (10%). This shows that though patients were taking more quantity of food but due to poor digestion resulting in Ama formation and subsequently vitiating Dosha and Dhatu resulting in the manifestation of different features.
Vyayama shakti
Avara Vyayama Shakti was found in majority of the individuals (52.22%) of this series. followed by 44.44% were having Madhyama Vyayama Shakti and 3.33% with Pravara Vyayama Shakti. This indicates that diabetic patients have lower exercise capacity due to abnormal increase of Meda Dhatu and decrease of other Dhatu like Mamsa, Asthi, Shukra etc.
Diet
Majority of the individuals (77.78%) were taking vegetarian diet and 22.22% individuals were taking mixed diet. this may be due to the traditional vegetarian dietary habits among the Hindu population who formed the greater part of this study.
Dominance of rasa in diet
Dominance Rasa wise distribution in the diet of 90 patients showed that Madhura (77.78%), Amla (45.56%), Katu (28.89%), Lavana (15.5%), and Tikta (20%).
Dominance of guna in diet
Dominance Guna wise distribution in the diet of 90 patients showed that Guru (86.69%), Snigdha (85.56%), Sheetha (58.89%), Ushna (41.11%), Laghu (13.33%) and Rooksha (14.44%). This type of Aahara will increase Kapha and Meda and causes Agnimandhya and Srotorodha which are the basic factors involved in the Samprapti of Prameha.
Dietary habits
Majority of the patients in the study were doing Vishamashana (51.11%) followed by Adhyashana (40%), Alpashana by 8.89% and Samashana by 2.22% of patient. This type of dietetic schedule results in Agnimandhya and Ama formation subsequently vitiating all the Dosha and Dhatu.
Job nature
Majority of the patients in the study were having sedentary nature of work (83.33%). This again supports the findings of previous researches that sedentary lifestyle is one of the important cause for DM.
Mental status
Majority of the patients in the study were having cheerful nature and devoid of worry (31.11%) followed, stressful (22.22%), anxiety (8.89%) and depression (12.22%). Achintana is an important cause for weight gain (Cha. Su. 22) on the other side stress, anxiety is known to cause endocrine disturbances resulting into metabolic disorders, In depression person is likely to overeat and will not involve in any physical exertion and may result into DM.
Results
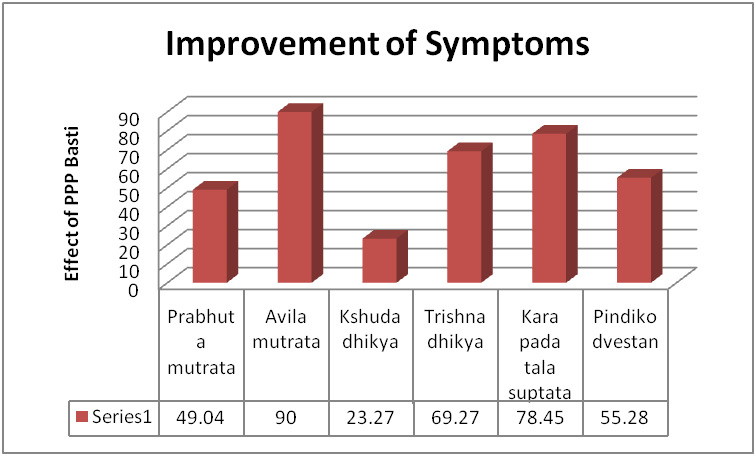
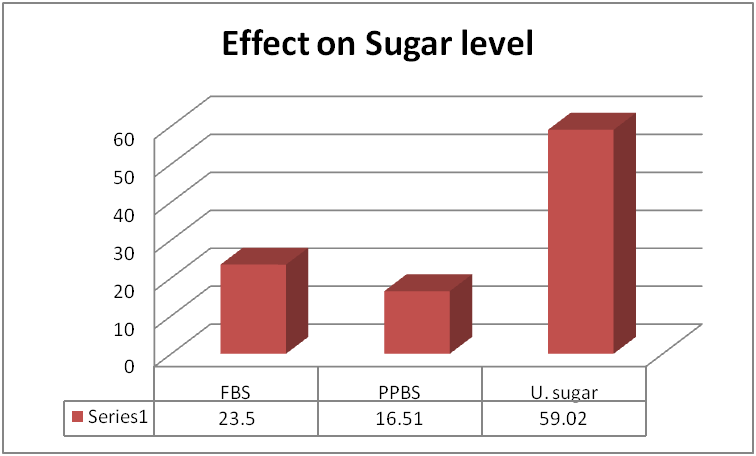
PPP Basti provided significant relief in the parameters of Prabhut mutrata (49.07%) Avila Mutrata (90%), Kshudadhikya (23.27%), Trishnadhikya (69.72%), Karapada Daha (41.77%), Ati Sveda (20.38%), Alasya (4.76%), Daurbalya (43.33%), Pindikodvestan (55.28), Klaibya (28.62), Nidradhikya (16.50%), BMI (3.74%), FBS (23.50%), PPBS (16.51%), Urine Sugar (59.02%), Serum Cholesterol (6.82%), Serum Triglycerides (4.74%), HDL (1.78%), LDL (9.91%) and VLDL (18.17%).
By PPP Basti moderate improvement was found in 26.66% of patients, 63.33% of the patients showed mild improvement and 10% patients remained unchanged
Statistical analysis
The data obtained on the basis of observation was subjected to statistical analysis in the term of mean, standard deviation error by applying the paired‘t’ test. The results were interpreted at p<0.05, p<0.01 and p<0.001 significance levels.
The effect of the PPP Basti on Madhumeha(type2DM) are presented in Table 7, Table 8 and Figure 1, Figure 2.
Table 5
Yoga-Ayoga-Atiyoga after Anuvasana Basti administration
|
Yoga |
Found in every Basti |
|
|
No. of Patients |
% |
|
|
Samyak Yoga |
30 |
100 |
|
Ayoga |
0 |
0 |
|
Atiyoga |
0 |
0 |
Table 6
Improvement in symptoms of Madhumeha(type 2 DM)
Discussion
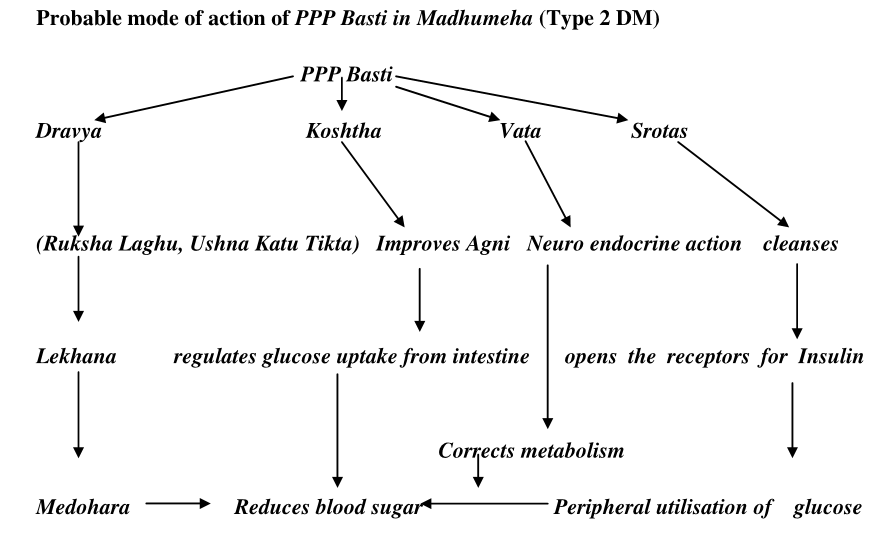
Acharya Charaka mentioned that Basti reaches the Nabhi Pradesha, Kati, Parshva and Kukshi expels out the Pureesha and accumulated Dosha after mixing with them.2 On the other hand Acharya Sushruta has clearly mentioned that though Basti is administered in the Pakvashaya, the active principles of Basti Dravya spreads all over the body through the minute Srotas in the same way as water reaches to all parts of the plant from its root.3
Honey being ambiphilic (lipophilic and hydrophilic) can dissolve both water as well as lipids in it. Salt will reduce surface tension and also converts gel form of honey to solution form. Then added oil will easily dissolve in to above mixture. Kalka will dissolve easily and will give potency to Basti Dravya. Kwatha will increase surface area for absorption along with its other actions. Temperature and continuous stirring will facilitate the above reactions. Finally the drug will attain colloidal form which is highly unstable, thus facilitating chemical exchange between large intestinal lumen and circulation through semi permeable membrane.
Absorption through the gastro intestinal mucosa occurs by active transport and by diffusion. So when a hyper osmotic solution is present in the lumen secretion towards it from the membrane and in presence of hypo-osmotic solution absorption from the solution occurs. It may be considered that Niruha Basti is hyper osmotic which facilitates elimination of morbid factors i.e. endo toxins into the solution and produces detoxification during elimination whereas the Sneha Basti and other nourishing Basti contain hypo osmotic solution facilitating absorption of active principles into the blood.
Enteric nervous system (ENS) normally communicate with the central nervous system through the parasympathetic (eg. via the Vagus nerve) and sympathetic (e.g. via the Prevertebral ganglia) nervous system. Sensory neurons of the ENS monitor chemical changes within the GIT as well as pressure of its wall. Enteric motor neurons govern contraction of GI tract smooth muscle and activity of GI tract endocrine cells. ENS also makes use of more than thirty neurotransmitters, most of which are identical to the ones found in CNS such as acetylcholine, dopamine, serotonine etc. The enteric nervous system has the capacity to alter its response depending on factors such as bulk and nutrient composition. As the total nervous system is interrelated so this regular stimulation to ENS may have some positive effect over the CNS also and in this way the neuro- endocrine regulation may take place.4
Basti corrects the Vata Dosha and by virtue of the lekhana property of the drugs used in PPP Basti it cleanses the channels removes the Medasa Avarana and regulates the movement of Vata.
Conclusion
The important findings of the present clinical study are presented below:
Sthula madhumeha a type of Prameha can be correlated to type 2 Diabetes mellitus based on sign and symptoms
Bahudosha, Agnimandhya particularly Dhatwagnimandhya, Medasavruta Marga, Margavarana Janya Vata Prakopa are important factors involved in pathogenesis of Madhumeha
Samshodhana is the first line of treatment for Sthula Pramehi.
Basti is best to correct Vata Dosha to remove the Avarana of Vata and PPP Basti is specially advised for Prameha, the drugs of PPP Basti are lekhana in nature their by reduces Meda and Kleda which are the basic factor in Prameha.
Triphala Taila for Anuvasana Basti which is dominant in Tikta, Kashaya Rasa, Katu Vipaka Ushna Virya, Kapha hara, lekhana and Rukshana action and proven for anti diabetic, hypolipidemic, and hypoglycemic action.
Percentage wise PPP Basti was better for Prabhutamutarata, Kshudadhikya, Karapadataladaha, Atisweda, Alashya, Sheetpriata, Pindikodvestana, Nidradhikya, Tamodarshan, Aavilmutrata, Karapada suptata, Dourbalya, Klaibya, BMI, Serum Cholesterol, HDL and LDL, FBS and VLDL.
PPP Basti was found better to reduce FBS.