Introduction
Defining itch
Itching is unpleasant cutaneous sensation which provokes desire to itch and this phrase is 200 years old. In any two week period, 8-9% of the population suffer from significant pruritus. Pruritus lasting more than 6 weeks is called chronic pruritus.1
Pathophysiology of pruritis
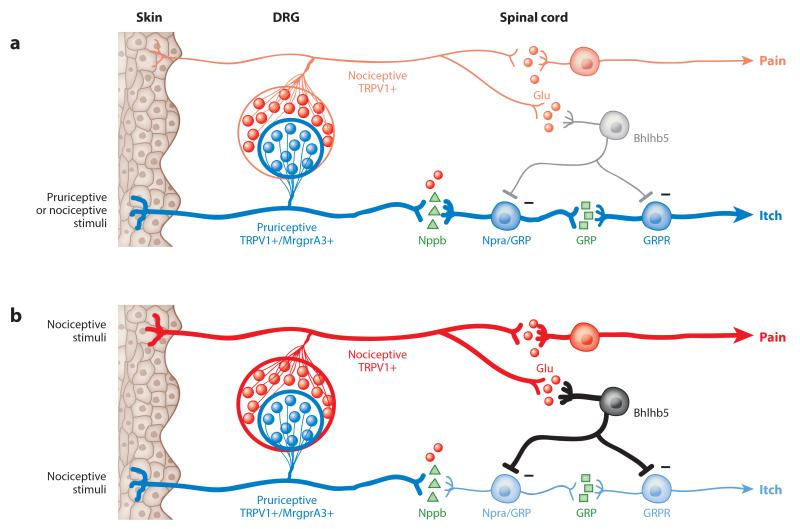
Pruritus is a complex process that involves the stimulation of free nerve endings found superficially in the skin. The sensation of pruritus is transmitted through the C fibers in the skin to the dorsal horn of the spinal cord, and then, via the spinothalamic tract to the cerebral cortex for processing. Many chemicals have been found to be pruritogenic, therefore causing the itch sensation, including histamine, serotonin, cytokines, and opioids. In addition to pruritogenic stimuli to the skin, itch can originate at any point along the afferent pathway. This may occur with neural damage secondary to stroke, trauma, or a space occupying lesion2 (Figure 1)
Exogenous itch triggers, exogenous pruritogens, and endogenous pruritogens secreted from immune cells (eg, mast cells, T-cells, eosinophils, neutrophils, and basophils) and epidermal keratinocytes stimulate small itch-selective unmyelinated C fibers in the epidermis and dermoepidermal junction. Itch-selective nerve fibers are divided into 2 subgroups: histaminergic nerves and nonhistaminergic nerves. Histaminergic nerves express the histamine type 1 (H1R) and type 4 (H4R) receptors, are activated by histamine, and are mainly involved in acute itch. Transient Receptor Potential Vanilloid type 1 (TRPV1).is acted by Capsaicin. GRP has emerged as a putative itch-specific neuropeptide restricted to nonhistaminergic itch. In human subjects, an intradermal injection of PGE2 elicits mild itching, whereas that of PGE2 enhances histamine- and serotonin-induced itching.3
Causes of Itch
Pruritus is distressing for patients and a challenge for clinicians to manage effectively. It is incompletely understood and is difficult to treat in many circumstances.
Table 1
Classification of itch based on disease state
If the diagnosis is unclear after the history and physical examination or if initial empiric treatment is ineffective, a limited laboratory evaluation should be performed, including complete blood count and measurement of thyroid-stimulating hormone, fasting glucose, alkaline phosphatase, bilirubin, creatinine, and blood urea nitrogen.4
Table 2
Screening in case of pruritus
Classification of Pruritus and Treatment Approaches
Chronic Urticaria (CU) is highly prevalent in the general population, and while there are multiple treatments for the disorder, the results obtained are not completely satisfactory. The second-generation H1 antihistamines remain the symptomatic treatment option of choice. Depending on the different pharmacokinetics and H1 receptor affinity of each drug substance.
The most widely used in application to CU have been the ethanolamines (diphenhydramine, clemastine), hydroxyzine, dexchlorpheniramine, and the more classical piperidines such as cyproheptadine, azatadine and ketotifen
Cetirizine was found to offer the most significant effect versus other antihistamines - the order of the inhibitory effect being as follows: cetirizine > epinastine > ebastine > fexofenadine > loratadine > placebo.5 Idiopathic itch is that which arises spontaneously and for which the cause is unknown.
Cholestasis
Pruritus is a complication of cholestasis including that associated with mutations in genes that code for transporters in the hepatocyte and from inflammatory liver diseases. In this regard, pruritus is more common in conditions characterized by bile duct inflammatory destruction and ductopenia including primary bile cirrhosis primary biliary cirrhosis (PBC) than in those characterized by hepatocellular injury such as chronic viral hepatitis. [Table 3]
Table 3
Uremic pruritus is common among dialysis patients. Effective treatments are not readily available. Desloratadine provides significant relief of uremic pruritus compared with no therapy. gabapentin has marginal efficacy. Gabapentin treatment is also for patients with generalized pruritus of unknown origin that is unresponsive to the usual treatment modalities. Evening primrose oil is rich in essential fatty acids such as linolenic acid that aids the body in reducing inflammation and is found effective for the treatment of uraemic pruritus.
The incidence of pruritus after intrathecal administration of opioids varies between 30-100% without large differences depending on the drug involved, being higher in the pregnant woman. The serotonin receptor antagonist 5HT-3, ondansetron (4-8 mg iv), has been shown to be effective in the prevention and treatment of this symptom, as well as the subhipnótic dose of propofol (20 mg, with or without infusion 30 mg/24h). Finally, butorphanol and nalbuphine (4 mg iv) that appears to demonstrate a greater effectiveness and should be considered the first-lime treatment,
Mirtazapine to be particularly effective in treatment of nocturnal pruritus. Mirtazapine has been reported to be effective in the treatment of itch associated with lymphoma
Facial neuropathic itch that progresses to scratching-induced ulcers is a condition known to dermatologists as the trigeminal trophic syndrome (TTS). Topical local anesthetics are often effective for even the most serve forms of neuropathic itch, and should always be considered.
The benefit of the other major topical therapy for neuropathic disorders, topical capsaicin, now available in concentrated 8% patches. Pimozide and carbamazepine for TTS, and gabapentin for brachioradial pruritus have found to be effective.
Drug-induced pruritus is a well-recognized adverse reaction, accounting for more than 10% of cutaneous drug reactions in previous studies. Some drugs such as opioids, antimalarials, and hydroxyethyl starch are known to induce itching without skin lesions. Pruritus with penicillin antibiotics and trimethoprim–sulfamethoxazole are thought to be secondary to inflammatory skin eruptions or cholestatic liver injury. Statin-induced xerosis cutis has been proposed as a potential mechanism of itch, with impaired barrier function resulting from decreased lipid distribution in the skin with inhibition of cholesterol biosynthesis. Other drugs are metformin, Beta blockers, Calcium antagonists, ACE inhibitors. Bronchodilators. NSAIDs etc.
Senile Pruritus. Elderly adults over the age of 70 years, generally suffer from this condition .
Oral antihistamines are effective if the pruritus is associated with an urticaria-like mechanism. Systemic corticosteroids may be effective if there is an inflammatory pathway suspected to be involved.
The immune system response to a food allergy ranges from mild rashes to abdominal pain to a life-threatening complication called anaphylactic shock. Lactose, a type of sugar found in dairy products. Gluten, a protein found in wheat, barley, and other grains. Skin symptoms include hives, tingling, itching, and redness. In babies with food allergies, the first symptom is often a rash. Antihistamics are useful for mild to moderate reactions.6
Table 4
General measures to reduce pruritis
Simple treatment with moisturisers can have a huge impact upon the intensity of pruritus by improving skin barrier dysfunction and reducing the entry of pruritogen for convenience, creams are usually applied during the day and greasier ointments at night. Calamine lotion is an over-the-counter (OTC). Calamine lotion, known for its antipruritic, anti-septic, and astringent properties, is a safe topical agent for the relief of itch and minor skin irritation. Its anti-itch property is attributed to its phenol content through its cooling effect upon evaporation from the surface of the skin.
Table 5
Topical therapies for pruritus
Topical capsaicin has been reported as useful for treating localised drug-induced pruritus.
The anti-pruritic effect of menthol has been described for lichen amyloidosis, as well as hydroxyethyl starch-induced, histamine-induced, and mustard gas-induced pruritus.
Topical corticosteroids are first line therapy for acute pruritus associated with moderate to severe inflammatory skin diseases, such as AD, allergic contact dermatitis, psoriasis andlichen planus. While the exact mechanism of action is not known, topical corticosteroids arethought to activate glucocorticoid receptors that inhibit cytokine activation.
Pramoxine is a local anesthetic agent that reduces neuropathic, anogenital and CKD-associated pruritus. It may also be combined with corticosteroids to reduce both inflammation and pruritus.
Topical strontium 4% hydrogel (a calcimimetic) has been shown to reduce both histaminergic and non-histaminergic induced pruritus. Strontium significantly reduced the peak intensity and duration of cowhage-induced itch when compared to the control itch curve.
Doxepin is a tricyclic antidepressant used to relieve itching from certain skin conditions (e.g., atopic dermatitis, eczema, neurodermatitis). It should be used only for a short time (no more than 8 days). Tricyclic antidepressants bind to H1 receptors with a high degree of affinity, and to a lesser extent to H2 receptors.
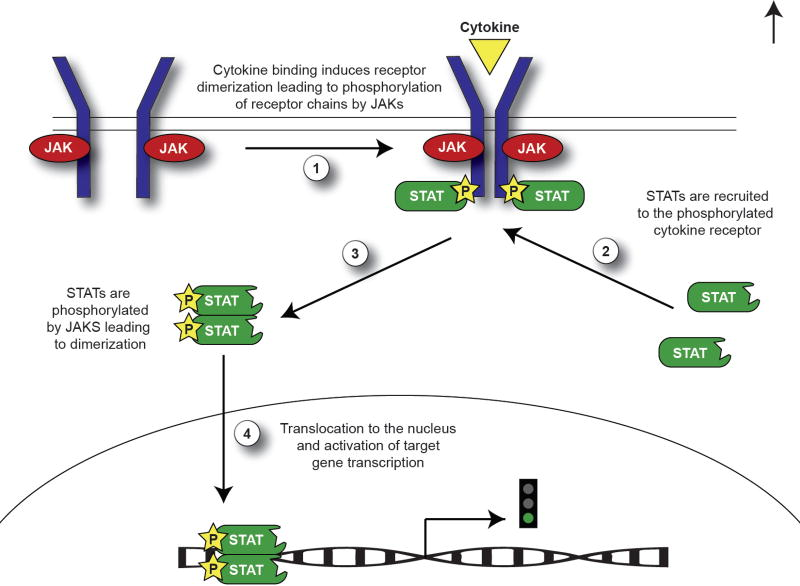
The underlying mechanisms of the ability of Topical calcineurin inhibitors (TCI) tacrolimus and pimecrolimus is to reduce pruritus are unclear and may be multi-factorial. TCIs regulate T-cell activation and inhibit release of various inflammatory cytokines. [Table 6]
Table 6
Topical vitamin D3 or its analogues, such as calcipotriol that has been used widely for the treatment of psoriasis, may also be useful to treat pruritus in some clinical scenarios.Vitamin D3 downregulates cellular adhesion molecule expression by inhibiting TNF-α mRNA expression and influences keratinocyte proliferation and differentiation. Topical vitamin D3 has also been reported to be effective in the treating the intensely pruritic lesions of prurigo nodularis. Topical vitamin D3 analogues have been shown to be safe and well-tolerated in a number of short-term and long-term clinical trials.
Oral Therapies for Pruritus
In cases of urticaria, sedative antihistamines, such as hydroxyzine, may be particularly valuable with pruritus during the night while non-sedating (second-generation) antihistamines such as loratadine, desloratadine, cetirizine and levocetirizine may be suitable in the daytime for relief of pruritus. In clinical practice, dose escalation with second-generation antihistamines has become commonplace for the management of patients with chronic urticaria who do not respond adequately to standard doses, provided potential benefits outweigh risks. The combination of H1- and H2-antihistamines has been widely used and studied in patients with refractory chronic urticaria. Coadministration of cimetidine significantly increased serum concentrations of hydroxyzine and improved suppression of wheal and flare. 50% of the patients responded with 90% or greater improvement within 10 days. Antihistamines have demonstrated poor efficacy in controlling Atopic dermatitis -associated itch. Oral fexofenadine and loratadine can be used with good results in chronic itch Antihistamines like diphenhydramine or chlorpheniramine are effective and since they cause sedation , they should be taken at bedtime. Sedation does improve quality of sleep in patients with itch.
The selective neuroepinephrine re-uptake inhibitor (SNRI), mirtazapine, has been reported to relieve itch in patients with advanced cancer, leukemia, lymphoma (including cutaneous lymphoma), chronic kidney disease, cholestasis and atopic dermatitis. Mirtazapine acts as an antagonist at noradrenergic α2-receptors and 5-HT2 and 5-HT3 serotonin receptors, increasing central noradrenergic and 5-HT1. Mirtazapine is given once daily due to its long half-life, which improves compliance. It may also improve insomnia, anorexia, and depression, all of which are common in advanced cancer, tapers intractable itch.
Gabapentin may be particularly useful in forms of neuropathic pruritus related to nerve entrapment disorders such as brachioradial pruritus and notalgia paresthetica. The use of gabapentin for neuropathic pain/pruritus is recommended only in patients over 18 years of age. The starting dose is 900mg/day (given as 300mg 3 times daily) and increased if necessary based on response. The maximum daily dose is 3600mg.
The oral immunosuppressants, cyclosporine and azothioprine, have demonstrated antipruritic effects in patients with atopic dermatitis most likely through their anti-inflammatory effects.
The κ-opioid receptor agonists butorphanol and nalfurafine appear to be beneficial in pruritic conditions. Butorphanol has been effective in the treatment of chronic intractable itch associated with inflammatory skin diseases or systemic diseases when administered intranasally at concentrations of 1 mg once a day. [Table 7]
Table 7
New Antipruritic Drugs
Aprepitant {tachykinin receptor antagonist}an NK1{neurokinin 1 receptor antagonist} inhibitor originally developed to treat chemotherapy induced nausea and vomiting , is effective for treatment refractory pruritus. Serlopitant has been used effectively in atopic dermatitis and chronic pruritis. Tradipitant is anovel neurokinin-1 antagonist that blocks substance P.
Butorphanol, both a µ-opioid antagonist and κ-opioid agonist, treats pruritus of varying aetiologies with high efficacy.
The newly approved oral drug nalfurafine hydrochloride (2.5 and 5 μg/day), a κ-opioid receptor agonist, has been proven to be safe and effective for the treatment of HD patients with uremic pruritus resistant to antihistamines. This drug suppresses itching and subsequently improves the mental condition of Haemodialysis patients.
Asimadoline is an orally active, selective and potent kappa-opioid receptor agonist with approximately 500-fold greater affinity for human kappa, as compared with either delta- or mu-opioid receptors, (used initially for IBS). a κ-opioid agonist is used for pruritis.
Crisaborole is a topical nonsteroidal phosphodiesterase4 (PDE4) inhibitor approved for the treatment of moderate to severe AD (Atopic Dermatitis). Applied as an ointment, crisaborole has proven to be effective in rapidly reducing pruritus in these patients.
Dupilumab has revolutionized the treatment of AD (Atopic dermatitis), significantly improving clinical symptoms of AD, rapidly reducing itch, and improving patients’ quality of life.
First Ascomycin macrolactam derivative to be developed for the treatment of inflammatory skin diseases, especially atopic dermatitis. It selectively inhibits the release of inflammatory cytokines. This derivative can only penetrate damaged skin.
Table 8
Doxycycline, an antibiotic, has shown antipruritic properties in the treatment of acne vulgaris. In addition to its ability to reduce inflammation, its antipruritic mechanism is most likely due to its attenuation of the PAR-2 (Proteinase-activated receptor) interleukin (IL)-8 pathway.
JAK inhibitors are commonly used in the treatment of inflammatory conditions such as rheumatoid arthritis. More recently, these medications are being investigated for use in chronic inflammatory skin conditions, such as AD and psoriasis. (Figure 2).
Baricitinib is not yet FDA approved, but is in clinical trials for rheumatoid arthritis (RA) (Phase 3),7 psoriasis, and atopic dermatitis.
Blockade of H4 receptors obstructs histamine-induced chemotaxis of eosinophils and mast cells. Antihistamines targeting the histamine 4 receptor (H4R), however, have shown some promise in treating itch. Thioperamide is an antihistamine at H3 and H4 receptors. Thioperamide behaves as both antagonist and inverse agonist, is being evaluated for itch.
Subcutaneous Ligelizumab therapy of 72 mg or 240 mg every 4 weeks is associated with greater control of chronic spontaneous urticaria symptoms, including hives and itch, compared with omalizumab. Ligelizumab has the potential to become the first-line treatment option in H1-antihistamine refractory chronic urticaria patients.8
Non Pharmacological Measures
UV therapy can be used to improve various inflammatory skin diseases, such as atopic dermatitis (AD); other eczematous skin reactions, psoriasis, lichen planus, pityriasis lichenoides; and cutaneous T‐cell lymphomas (eg mycosis fungoides or Sezary‐syndrome) or urticaria pigmentosa, the cutaneous variant of mastocytosis. Many UV‐responsive skin diseases are accompanied by chronic pruritus, and phototherapy can both be used to improve the skin lesions and reduce chronic pruritus. 9
Wet wrap therapy is a relatively safe and effective intervention in atopic dermatitis. It is a treatment modality using a double layer of tubular bandages or gauze, with a moist first layer and a dry second layer.
Adding sodium hypochlorite or bleach to bath water has shown to reduce the Staphylococcus aureus counts and hence the severity of atopic dermatitis and frequency of its relapses
The psychological intervention and behavioral therapy in atopic dermatitis are aimed at breaking this itch-scratch cycle. Psychological stress can alter permeability barrier homeostasis and stratum corneum integrity, justifies the reported exacerbation of atopic dermatitis in 30% patients following stressful situations. 10
Conclusion
Chronic itchy skin is a universal symptom of most types of eczema. Itch from eczema is different than itch from a bug bite Because of this, common medications used for itch, such as antihistamines, do not work well on the itch associated with eczema. At present, there is no universally accepted therapy for itch. Treatment for chronic itch includes corticosteroids, antihistamines, and systemic therapies such as naltrexone, gabapentin, UV light therapy, and immunomodulatory treatments Itching can occur as chronic side effect of anti-cancer treatments including (Interleukin-2), Interferon radiation therapy, acute and chronic graft-versus-host disease (GVHD), and occasionally supportive growth factors including (G-CSF) and (GM-CSF). Steroids work by reducing inflammation. Antihistamines reduce symptoms of an allergic reaction, such as rash, hives and shortness of breath. Itch in AD is multifactorial, combining therapies can be a useful approach to management. In general, elimination of trigger factors and psychological/behavioral interventions can be combined with any other therapies.