Introduction
On March 11, 2020, the World Health Organization (WHO) proclaimed COVID-19 to be a pandemic after it affected 114 countries in three months, infecting over 118,000 people.1 Till date, nearly 153 million people have been infected worldwide and more than 3.2 million deaths have been reported. In India, a total of more than 19.9 million cases have been reported so far and more than 219 thousand people have died.2 The second wave of COVID-19 in India, has been even more alarming as the COVID-19 cases started rising in February 2021, when India reported an average of about 10,000 infections a day. The situation worsened progressively in April 2021, ending the month by setting new global records for daily cases. India has reported nearly 7 million new cases in the month of April.2 According to WHO one in three new corona viruses cases globally are being reported in India.3 As of now this second wave does not seem to be slowing down.
The second wave of the pandemic in India has put immense pressure on the existing health infrastructure with an unprecedent demand for hospital beds, oxygen supply, medicines, ICU beds and need for vaccination facilities. Government of India and the State Governments have been taking unprecedented regulatory measures to address these challenges. These measures range from simple advisory to state-imposed lockdowns and curfews, price capping, vaccination campaigns, strengthening the infrastructure for testing and treatment, and public health measures.
In the midst of all the focus on the containment of COVID-19 infection, chronic diseases like cancer characterized by continuity of care have taken a backseat. In this paper, we review the impact of COVID-19 on utilization of cancer care services, the negative effect on cancer outcomes due to delay and discontinuity in treatment and what alternative measures can be taken to maintain the continuity of cancer care in COVID-19 times.
Decreased access to cancer care during Covid-19 pandemic
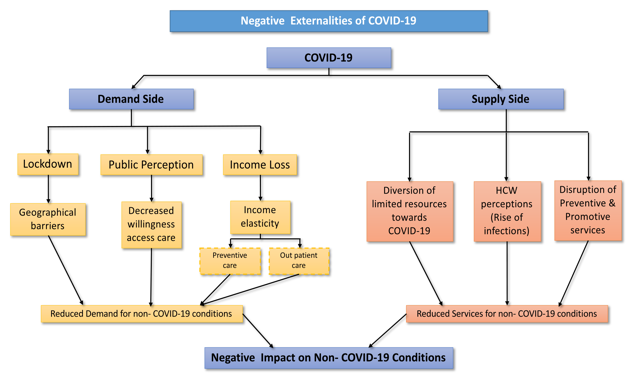
As urgent takes precedence over important, the entire system focused on prevention, diagnosis, treatment and containment of COVID-19 infection is likely to miss opportunities for timely diagnosis and treatment of other diseases. Various factors are responsible for decrease in access to cancer care during the COVID-19 pandemic (Figure 1). In the context of delivery of treatment for cancer, usually at regional cancer centres which are localized in urban areas, lead to problem of access due to state imposed lockdowns and curfews. The latter impose geographical barriers to access services for curative care, specially for the economically weaker sections. As a result, lockdowns to prevent transmission of COVID-19, create supply and demand side barriers to access routine health services.
Secondly, the COVID-19 outbreak has also placed unprecedented demands on the health system. Existing human resources, diagnostics, hospital beds, intensive care units and other health care infrastructure is being allocated to activities for COVID-19 response.4 Majority of referral centres across the country have shut down their physical outpatient care and elective medical or surgical procedures. Diagnostic services have been dedicated to the covid care. Majority of health care workers have been posted for COVID-19 care. Moreover, due to communicable nature of the disease, healthcare providers — both implicitly and explicitly — reduced provision of care for non COVID conditions, citing concerns for safety of healthcare providers as well as reducing community transmission in hospitals. As a result, the routine cancer services have been compromised.
Thirdly, requirements of physical distancing and reluctance to visit health facility due to fear of being infected, results in poor care-seeking for routine conditions by patients as well.5 Patients of chronic disease, being wary of going out, or facing difficulties in movement due to lockdown restriction or non-availability of facilities for non-COVID-19 conditions, might miss on treatment, ending up with long-term sequelae. In an analysis carried out at our department, a tertiary care centre for cancer delivery in north India providing services which include, outpatient care, hospitalization, radiation therapy, chemotherapy and palliative care. Annually, it caters to a total of nearly 26,000 outpatient visits, 5500 hospitalizations, 800 patients treated on radiation therapy machine, and 8000 day-care visits for chemotherapy. Prior to the onset of COVID-19 restrictions, 89 outpatients visited daily, 58 patients got radiation treatment and 10 patients were hospitalized for cancer care per day. Following COVID-19 restrictions, the estimated number of OPD patients and patients receiving radiation therapy dropped abruptly by 66% (58 patients and 91% (53 patients) per day, respectively. The decline in number of female and male outpatient attendance was 79.5% and 51%, respectively. The reduction of outpatient care for the various sites was highest for breast cancer (100%), cervical cancer (76%) and head and neck cancer (54%).6 A similar reduction in outpatient care was seen at a tertiary care center in North East India (50%)7 and the country’s largest cancer center in Maharashtra (65%).8
As quoted in the data above, the worst affected in terms of decreased access to cancer care are the females. This is again highlighted by various other data9 in view of the challenges faced by the females in access to various health care services like antenatal care, lactation support, postpartum depression, cervical and breast cancer, abortion services, other gynecological and menstrual disorders and various other medical conditions unique to women.
Effect due to loss of continuity of cancer care
Analyses from the 2014-2015 Ebola outbreak suggests that the increased number of deaths caused by measles, malaria, HIV/AIDS and tuberculosis attributable to health system failures exceeded deaths from Ebola.10 Particular attention needs to be paid to provide continuity in the delivery of essential health care for chronic diseases like cancer, tuberculosis, dialysis for chronic kidney disease, child and maternal services, diabetes, hypertension, cardiac diseases, etc, while managing the pandemic.
Oncology services are marked by a continuity of treatment in both curative and metastatic disease where life years and better quality of life can be added. All oncology treatments are directed with the aim to start at the earliest, finish with minimal or no gaps, restart after any interruption and compensate for missed treatment. Any significant gap, interruptions, delay or inability to get timely treatment impacts loco-regional control and survival in cancer patients.11 A study on the impact of COVID-19 on outcomes for patients with cervical cancer in India estimated an increase in deaths of 2.52% (n = 795) to 3.80% (n = 2,160) caused by cervical cancer with treatment restrictions ranging from 9 weeks to 6 months, respectively, as compared to no delay. On the contrary, 88-238 deaths because of COVID-19 disease were saved during this restriction period among the patients with cervical cancer. Overall, the excess mortality because of cervical cancer led to 18,159-53,626 life years being lost and an increase of 16,808-50,035 disability-adjusted life-years.12
Equally, important are the community based screening programmes for the most common cancers in the country like breast cancer, cervical cancer and oral cancers which facilitate the early diagnosis of these cancers. COVID-19 has adversely affected this community based screening leading to late or missed diagnosis with patients presenting in advanced stages and subsequent poor outcomes.
Regular follow up with the oncology team for cured patients is an essential part of cancer care so that timely diagnosis can be made of any recurrent disease that can be salvaged to give another opportunity for cure in these patients. Many patients, on maintenance treatment for cancer need to follow up with the oncology teams for disease assessment and drug procurement, which may continue for many years. Patients on opioid drugs for pain management also depend on their visits to the tertiary care centres as these opioid drugs are not available over the counter. Loss of continuity in all these cancer services due to COVID-19 adversely affects these patients.
Measures to provide continuity in cancer care
This pandemic has brought with it many unforeseen implications for health care. Globally no country was prepared to handle a pandemic of this scale. The level of spread of infection resulted in placing unprecedented priority for COVID-19 prevention and mitigation, which has had its negative externality in terms of poor access for other services.5
Cancer is a chronic disease, and by virtue of its nature it demands a continuity of care whether it is for patients undergoing screening, diagnosis, ongoing treatment with any modality (surgery, chemotherapy, radiotherapy, targeted therapy, palliative care or follow up). Any disruption in this continuity can adversely impact treatment outcomes
As the pandemic continues, healthcare systems must balance the need to provide necessary services while minimizing risk to patients and healthcare personnel. Cancer care, often involves immunosuppressive therapy like radiation, chemotherapy, tumour resection and inpatient treatment. During early part of the pandemic, majority of the oncology treatments were either deferred or postponed. However, the situation of the pandemic continued to worsen over the passing days. The oncologists realised that this infection is here to stay and cancer patients cannot be deprived of life saving procedures for long. So, oncology centres across the country decided to provide services to cancer patients with utmost caution, safety measures for health care workers and patients and appropriate modifications of the treatment schedules, prioritizing patient needs based on the disease status during these challenging times.13, 14, 15
In the immediate term the aim is to provide oncology services, safeguarding the spread of infection in the patients and health care providers. All patients and health care workers (HCW) should be triaged and screened at the entry point of hospitals. Masks, thermometers, hand rubs should be made available at entry points and any suspects should be referred to screening OPDs.13, 14, 15, 16, 17 Outpatient consultations should be spaced out and patient number capped to prevent crowding in the waiting area with prior online appointment. Strictly, only one attendant should be allowed with the patient. Personal protective equipment should be made available to HCW involved in aerosol generating procedures18 and regular sanitization of the patient waiting areas, treatment areas and working areas should be done13, 14, 15, 16, 17 In addition, another important intervention which needs to be scaled up is the vaccination against COVID-19. The COVID-19 vaccination has already been given to health workers, those above 45 years and with a comorbidity, as well as is now being currently made available for young adults between the age of 18-45 years. Those with cancer are also in the category of those who are entitled for vaccination. This should be further encouraged to remove any vaccine hesitancy.
In the medium term, aim should be to provide a continuity of cancer services in the existing prolonged state of the pandemic. All HCW should be performing duties on a rotational basis so that only a group of HCW are exposed during a particular period. In an event of positivity amongst the working cohort, it ensures that the other lot takes over and the service provision is not shut down.13 Departments should develop protocol in advance on how to deal with shortage of staff if 10% of the existing staff is sick or even one third or one half of the workforce is unavailable. Patient treatment should be prioritized based on the nature, stage and expected outcome of the disease.19, 20, 21, 22 Oncologists should revise chemotherapy protocols to minimize both the frequency of chemotherapy visits and the degree of immunosuppression. Cancellation of elective surgeries, in view of diversion of HCW and resources to COVID-19 services should lead to patients being offered systemic treatment (chemotherapy and or hormone therapy) as bridge therapy or being shifted to radiation treatment.20, 21 Radiation for cancers like breast, prostate, endometrium may be postponed as per the current institution waiting period while radiation for cancers like cervix, head and neck cancers, lung cancers may be started on priority, albeit with modified hypofractionated schedules.18, 19, 20 Departments may have to refrain from the most complex treatments and accept more standard techniques. Patients on palliative treatment should be shifted to oral metronomic therapy. Most of these modifications may not affect long term outcomes.19, 20, 21 All patients requiring admissions, injectable chemotherapy, radiotherapy or surgery should be tested for COVID-19 prior to the intervention to curtail any spread of infection among the HCW. Oncology treatments should be deferred for COVID-19 positive patients and treatment resumed once the COVID-19 test is negative and these patients are declared non-infectious.23, 24 This prevents spread of infection to other HCW and immune compromised other patients. Also, the complications of COVID-19 infection on patients on active oncology treatment may be manifold.25 All asymptomatic follow up patients are being encouraged to follow up telephonically through the telemedicine services available.26 All multidisciplinary interactions for patient care discussion or academic learning should be held on a virtual mode.
In the long term, learning from this pandemic should help us aim to modify the health delivery system with more involvement of the primary health services who work in integration with tertiary care centres to provide continuity of care for chronic diseases. In the midst of the pandemic, Ministry of Health and welfare, in collaboration with NITI Aayog — the policy think tank of Government of India, released Telemedicine Practice Guidelines27 enabling Registered Medical Practitioners to provide healthcare in remote settings using telemedicine. These guidelines recognize telemedicine as an enabler of healthcare access and affordability through faster access to appropriate interventions and access to services that may not otherwise be available. There have also been frequent online training sessions for nurses, paramedic staff and primary health workers for protocol to be followed during these teleconsultations. Increased use of technology and opening up telemedicine through transparent guidelines will improve access to healthcare even in remote locations in geographically diverse country like India.28 To prevent delay in treatment, initial diagnostic workup like examination, biopsy and basic radiology may be carried out at peripheral health centre in collaboration with the experts at the tertiary care centre, so that treatment can be initiated as soon as the patient reaches the tertiary centre. The list of providers and facilities allowed to administer chemotherapy remotely may be expanded. Patients on treatment with oral therapies, could be provided up to three months medicine supplies at a time as prescribed by medical officers, provided patients are stable. Patients may be advised to contact community health officers where available, or medical officer at primary health centre, in case of any complications and teleconsultations with treating centres as required. Following the pandemic too, all tertiary care centres should run regular telemedicine services with helpline numbers. Health Department may issue directives to the district administration coordinated by the PHC team for providing referral transport on fixed periodic basis to patients with chronic diseases to allow easy movement of cancer patients to access care from their respective tertiary centres. Mobile Medical Units could be utilized on a regular basis for delivery of services, especially screening facilities, follow-ups, end of life/ palliative care and delivery of drugs. On a regional and national level, departments should inform each other of their developments and experience to combat the crisis better.
Conclusion
The ongoing COVID-19 pandemic has exposed our unpreparedness in dealing with this kind of crisis which was never foreseen. We need to learn a lesson from this pandemic to prepare our health sector for the current existing crisis and any future pandemics that may affect our health system. In view of the prolongation of the pandemic we should try our best to ensure continuity of oncology therapies while protecting patients, care givers, health workers and community as a whole. Negative outcomes can be minimized through the concerted efforts of healthcare providers and regulatory bodies, individual clinicians and patients. The primary health care system needs to be strengthened and integrated with the existing tertiary care centres to be able to provide a continued access to specialized services.