Introduction
Anal fissures, ranging from linear to oval, result from a longitudinal tear in the anal canal below the dentate line. 1 Described by Lockhart-Mummery in 1934 2, they can be acute, causing pain and bleeding, or chronic, persisting for more than 6 to 8 weeks, with distinct symptoms like exposed anal sphincter fibers, hypertrophied anal papilla, and skin tags. 3
Most common anal fissures occurs posterior to the anal sphincter (Greater than 75%-80%). Less than 25% of anal fissures occur in anterior position and these anterior anal fissures are most commonly seen in females. Less than 1% of anal fissures are seen in midline. Based on the duration of symptoms the anal fissures are classified into acute and chronic. Though few old research articles has mentioned 8 weeks as this duration, the latest reviews and researches has suggested that any anal fissure that persists more than 6 weeks are considered to be chronic in nature. 1
Secondary anal fissures can be attributed to a more systemic clinical condition like Crohn’s disease, HIV, Anal Cancer, Syphilis, Herpes and Ulcerative Colitis. 2 Pain was relieved as well as the fissure healed without recurrence after spasm relief. The surgical approach has traditionally been the preferred approach for treating spasms. For fissure most commonly utilized effective techniques whichare following:anal stretch, open lateral sphincterotomy, closed lateral sphincterotomy, posterior midline sphincterotomy as well as to a reducedlevel of dermal flap coverage of the fissure.
Incontinence-related to the rate of disease in a population from these processes, which were previously believed exist highly uncommon, 4 has recently been reported to be significant, 5 which has increased interest in therapy without sphincter division.
Drugs like GTN and ISDN increase blood flow, resulting in over 80% healing rates in sphincterotomy. However, topical GTN's effectiveness is inconsistent, with healing rates varying from 40% to 69%, possibly influenced by the duration of patients' complaints; those with a history exceeding 6 months are less likely to heal. 6
In previous studies, conservative treatments in Ayurveda have also been described. Anal fissure is a prevalent anorectal issue in the Saurashtra region, primarily attributed to the escalated consumption of spicy foods like Ganthia and Bhajia (deep-fried items), leading to constipation. This condition manifests as a newly formed linear ulcer in either the anterior or posterior part of the anal canal, prompting patients to seek prompt relief from the intense burning pain associated with it. Parikartika is considered a SadhyaVrana in this context.The ancient text, SushrutaSamhita Sutra Sthana, advocates the use of YashtimadhuGhrita to alleviate immediate pain in fresh wounds. However, despite its historical recommendation, there is a notable absence of research on the efficacy of YashtimadhuGhrita in managing Parikartika (acute fissure-in-ano) to date. 7
In a previous study conducted by In a study by Patel et al. 7, YashtimadhuGhrita was compared with conventional lignocaine–nifedipine ointment for treating acute fissure-in-ano in 36 patients. Group A (YashtimadhuGhrita) showed a slightly longer time for pain relief but faster healing of anal ulcers compared to Group B. Both groups had similar timelines for relief from bleeding per rectum. However, YashtimadhuGhrita led to a more complete remission of Parikartika symptoms. The study concluded that both interventions were equally effective in providing symptomatic relief in acute fissure-in-ano. Limited data is available regarding the effectiveness of different treatments and their respective rates of rapid healing. 7
The purpose of this review was to estimate theimpactof duration of initial symptoms on the response of acute and chronic anal fissures to conservative treatment and to demonstrate how acute as well aschronic anal fissures respond to conservative treatment.
Materials and Methods
We conducted a literature search of publications that had been published in PubMed Medline, the Cochrane Library as well as additional sources (Google Scholar, clinicaltrails.gov) from year February 2012 to September 2021. This review was conducted in peace with the PRISMA Statement and the Cochrane Handbook for Systematic Reviews of Interferences. To find randomized controlled trials (RCTs) evaluating different anal fissure treatment techniques published between 2012 and 2021, we carried out a thorough the searching the literatures by utilizing databases. The following search terms were utilized to look for papers that were written in English: Anal fissure, Fissure in Anal and conservative treatment, symptoms of anal fissure, anal fissure and GTN, Anal fissure and Botox, Anal fissure and pathophysiology, anal fissure and calcium channel Blockers, Pathology and Physiology. After screening the titles appropriate abstract were taken. Additionally, the reference lists of each qualifying journal were checked for additional prospective papers.
Only RCTs that observed at anal fissure treatment alternatives were taken into account.
Inclusion criteria’s: (a) Researches that have studies the periods of symptoms of anal fissure, (b) Reporton signs of anal fissure and its impact on response to conservative treatment, (c) English texts,
Exclusion criteria
Atypical fissures which occur due to conditions like cancer, anal infection and inflammatory bowel disease were excluded. All the articles and literature other than in English language are excluded.
The following information was taken from the selected publications: year of publication, country of study, number of patients, location of fissure, time of onset, intervention utilized, time at follow-up, healing of fissure, complications and recurrence. To eliminate selection bias, two investigators separately entered all data, which were only compared at the end of the reviewing procedure. A 3 rd author finally reviewed the database. Repeated articles were removed as well as the inconsistencies clarified. The statement of PRISMA as well as Cochrane Handbook for systematic reviews was followed when doing the statistical analysis.
Description of studies
The present systematic review yielded 1048 articles on initial search; first 614 duplicate publications were removed. After screening additional 467 articles were excluded because of some parameters are missing in articles and also somearticles are incomplete and irrelevant with present study. 147 full articles were assessed for the study. After performing complete screening and analyzed data a total 14 studies were involved in this systematic review. The articles ranged in date from 2012 to 2022.
13 RCTs have documented 49 distinct comparisons of the anal fissure healing efficacy of medicinal treatments. Seventeen agents were utilized which are as follows: (nitroglycerin ointment (GTN), isosorbide mono & dinitrate, Botulinum toxin (Botox), diltiazem, nifedipine (Calcium channel blockers orCCBs), hydrocortisone, lignocaine,indoramin, clove oil, L-arginine, sitz baths, sildenafil, "healer cream" and placebo) and Sitz baths anal dilators and surgical sphincterotomy.
Patient characteristics
89% of patients with acute anal fissure treated with THD as well as 80% with GTN were demonstrated efficacy, at 6 weeks.
According to Nelson RL,et al.8 analyzed that the 48.9% of patients exhibited efficacy with .2% GTNverses placebo in acute anal fissureGTN was considered to be slightly, in spite of thatextensively more effective apart from a placebo inhealinganal fissure (48.9% vs. 35.5%), in spite of that late recurrence of fissure was frequent, occurring in up to 50% of individuals who were first cured.
Chronic anal fissure that is persistent 63.8 % of patients in the selected trialsdisplayed efficacy with topical nitrates, 100% with botulinum toxin, 46 % with diltiazem and 69.22 % with GTN,46% with Diltiazem (DTZ),62.8% of patients in the selected studies showed efficacy with THD treatment in chronic anal fissure at six week At 8 weeks,96.80% of patients in the selected trials showed efficacy with GTN therapy, while 95.13% of patients showed efficacy with Botulin in chronic anal fissure.
At 3month,100% of patients in the selected trials showed efficacy with GTN in chronic anal fissure.
At 6month, 98% of patients in the selected trials showed efficacy with GTN in chronic anal fissure.
At 12 month, 86%of patients in the selected trials determined efficacy with Botulin toxine treatment and 93.3% with DTZ (Table 1).
Table 1
Master chart showing the efficacy of different conservative treatment approaches as reported in medical literature and researches
|
Author |
Year |
Nature of ulcer |
Duration |
Treatment |
Efficacy |
Recurrence |
|
Nelson RL,et al. 8 |
2012 |
Acute &chronic |
NS |
.2%GTN,Placebo |
48.9%GTN |
50% |
|
35.5% Placebo |
||||||
|
AlaaMagdy,et al. 9 |
2012 |
Chronic |
6month |
.2%GTN Ointment. |
98% |
2% |
|
Sajid M. S,et al. 10 |
2013 |
Chronic |
NS |
.2GTN/ diltiazem 2% |
95% |
NS |
|
AlaS,et al. 11 |
2012 |
Chronic |
6 weeks |
.2%GTN/diltiazem 2% |
91.66% |
NS |
|
LatifA,et al. 12 |
2013 |
Chronic |
3months |
.2% GTN |
100% |
NS |
|
RidzuanFarouk,et al. 13 |
2014 |
Chronic |
8 weeks |
GTN/diltiazem 2% &Botox |
96.80% |
6.20% |
|
HosseinGandomkar,et al. 14 |
2015 |
Chronic |
12month |
Botulin Toxin/2% Diltiazem |
86% |
NS |
|
R. Digennaro,et al. 15 |
2015 |
Acute |
Aft 40days |
THD Levorag_ Emulgel |
89.4 % Acute |
NS |
|
62.8% Chronic |
||||||
|
Emile SH.et al. 16 |
2017 |
Acute/Chronic |
6 week |
.2% GTN |
80% Acute |
NS |
|
40% Chronic |
||||||
|
Matthew Z. Wilson,et al. 17 |
2018 |
Chronic |
Per day |
High fiber diet – 25-35 grams |
81.2% |
NS |
|
VenkateshS.,et al. 18 |
2019 |
Chronic |
6week |
.2% GTN/ 2% Diltiazem |
76%GTN 46%DTZ |
NS |
|
Carlos Walter SobradoJúnior,et al. 19 |
2019 |
Chronic |
12months |
2% diltiazen |
93.3% |
0% |
|
P. A. Boland,et al. 20 |
2020 |
Chronic |
8week |
botulinum toxin |
95.13% |
6.9% |
|
|
||||||
|
6.9%SP |
||||||
|
D’Orazio,et al. 21 |
2021 |
Chronic |
40days |
Botulinum Toxin/ nifedipine & lidocaine ointment |
100% |
7.3% |
Emile SH et al 16 has conducted an exclusive study on the period of indications of anal fissure and retaliation to conservative therapy and established a very reliable connection between both the prospects. In their research article a 6 week conservative therapy has been applied for a group of 60 cases with both acute and chronic anal fissures. The conservative therapy used in the study are Bulking agents, Sitz baths and 0.2% GTN. A visual analog scale and Wexner constipation score were used to measure the pre and post treatment outcome.
The results clearly indicate that the patients had their symptoms reduced and healing is promoted in cases with acute anal fissures than in cases with chronic anal fissures.It is also has been mentioned that the healing rate has been dropped down from 100% to a drastic 33.3% for patients with symptom duration of more than 6 months.
Figure 2
Flowchart for the new systematic review underPRISMA 2020, which simply searched databases and registrations.

The presence of sentinel tag , fibrosis of anal spinchter thus reducing the absorption of conservative treatment modalities has been attributed for the reduction in healing rates in patients with chronic anal fissures.
Table 2
Adapted from Sameh Haney et al. 16
Healing took place in 33 of 36 (91.66%) patients were treated byusing the DTZ after 6 weeks as well as 15 of 25 (60%) cases were medicated with Glyceriltrinitrate after 8 weeks, indicating a significantalteration in favor of Diltiazem in the chronic anal fissure, according to Ala S et al. 11 The remaining patients either exhibited non-compliance or failed to recover, necessitating surgery. In patients receiving Diltiazem, other adverse effects also occurred less frequently. Glyceril gel is inferior thanDiltiazem gel since it has a much slower healing rate and more side effects.
By the end of 6 weeks, the study by Venkatesh S. et al. 18 found that 80% of cases inside the DTZ group and 76% of caseswithin GTN group had fully healed the fissure. In the DTZ group, 14% of patients reported having a mild headache, but 46% of individuals in the GTN group reported experiencing a similar condition. For chronic anal fissure, topical 2% DTZ considered to be the preferable first-line approach of chemical sphincterotomy with the less side effects.
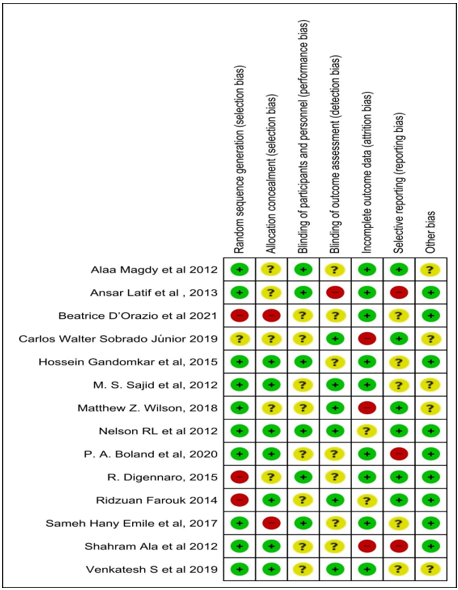
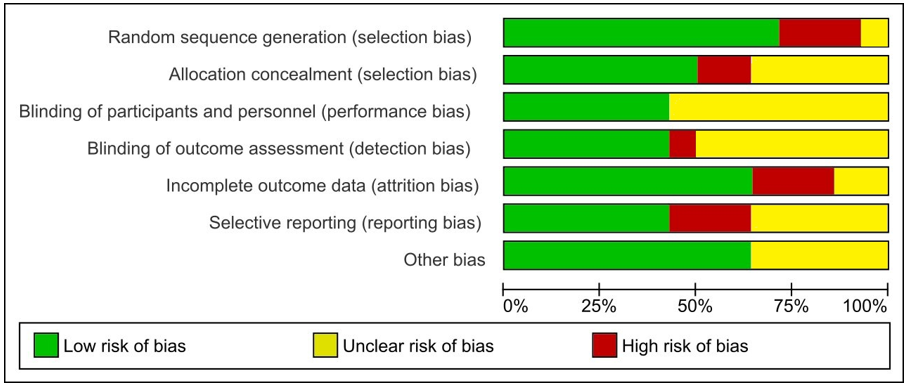
Risk of bias assessment
The risk of bias was evaluate for RCTs utilizing the Cochrane collaboration tool and performed using the RevMan software. It was determined whether a risk assessment domain was considered high, unclear or low risk (selective reporting) depending on the selection bias (random sequence generation and allocation conc`ealment), performance bias (blinding), detection bias (assessor blinding), attrition bias (incomplete outcome data), and reporting bias.Therefore, based on the domains and criteria, the whole risk for each study was rated as low, unclear or high risk. The risk of bias assessment for the 14literatureswereinvolved in the present study which, is shown in Table 2. All trials had significant methodological flaws for at the minimum one bias dimension.Insufficient/unclear arbitrarily (high risk in 12.24% of the experiments) and blinding of results evaluators (unclear in 33.67% of the trials) had the most problematic domains. The studies that specified allocation concealment (low risk in 54.08%).
Figure 3
The proportions across all involved papers represent the risk of bias graph-review authors' calculations of each risk of bias item.
Discussion
The anal fissure is one of the most common causes of pain and bleeding in the anal area.It is classically divided into acute and chronic with a period of symptoms of 6 weeks or more being the determining factor.16 It is believed that passage of a hard bowel motion can inflict a minor tear in the anoderm and an acute ulcer can result. This will usually heal quickly with no long-term sequelae. Failure of complete and early healing of this initial ulcer can lead to sustained internal sphincter spasm and occasionally progression to a chronic anal fissure.22
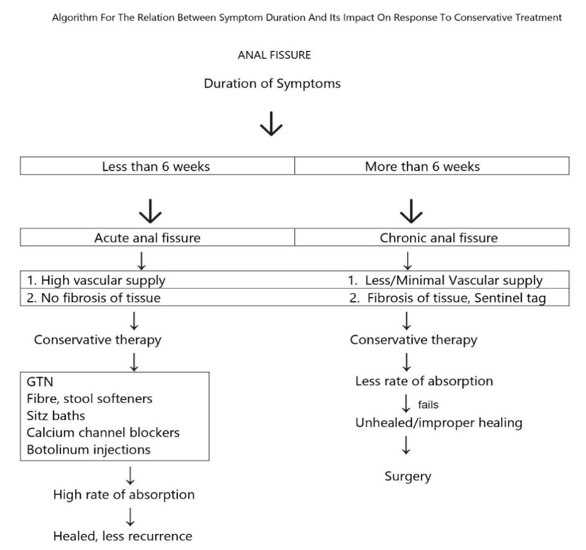
Duration of Symptoms Figure 5
Medical/ conservative management which includes Fiber in food , stool softeners , sitz baths,23 topical nitrates calcium channel blockers and botox injections either solitarily or in conjugation has remained the first line of therapy for treatment of acute anal fissures. The main mechanism of action includes the decrease in pressure if internal anal sphincter leading to vasodilatation followed by increased blood flow to the sphincter muscles thus promoting healing.
However this is not in the case of chronic anal fissures or with anal fissures with prolonged symptom duration. The main reasons attributed for this decrease in healing rates when conservative treatment modalities are used are the presence of a sentinel tag or fibrosis of anal sphincter muscle tissues thereby interfering in the absorption of topical agents especially GTN . As mentioned in the cohort study by Emile SH et al. 16 the healing rates has been decreased by 100% to 33.3% as the duration of symptoms prolong.
Abnormalities of the inneranal sphincter (IAS) has been described in association with both acute and chronic anal fissures. 24 While an acute anal fissure is associated with functional spasm of IAS, chronic anal fissures are related with both sphincter spasm and a degree of hypertrophy and secondary fibrosis. 25 The IAS hypertrophy accompanying chronic anal fissures further compromises the already deficient blood supply of the posterior anal commissure that is why Schouten and colleagues. 26 proposed that chronic anal fissures are essentially ischemic ulcers that do not heal spontaneously for several months.
Medical treatment is the mainstay for management of acute anal fissures as 80% of them resolve completely with conservative treatment. 24 On the other hand, healing of chronic fissures range between 8 and 52% after stool softeners and local anesthetic agents, and between 40 and 69% after topical GTN ointment with recurrence rates up to 50%. 26 Whereas, The healing of anal fissures is characterized by the absence of symptoms and the presence of granulation tissue in the fissure bed. According to a randomized clinical trial by Gough and Lewis, 43.6% of patients experienced fissure healing with a 2% lignocaine topical application for one month. 27 Shub et al.'s retrospective study reported a 44% healing rate within 4–8 weeks of conservative treatment. 28 Additionally, Perrotti et al. found that the local application of nifedipine and lidocaine gel led to fissure healing in 94.5% of patients within 6 weeks. 29 In our observational group, the fissure healing time was determined to be 1.5 ± 0.5 weeks.
So based on the literature reviews it can be said that conservative treatment modes for the treatment of anal fissures are directly linked to the duration of symptoms. The lesser the duration of symptoms the higher the rate of healing is proved by the 60 patient study by Emile SHet al 16 The same theory holds good for the recurrence rates of anal fissures too.
The majority of anal fissures can be effectively treated with conservative management, involving sitz baths, laxatives, a high-fiber diet, and topical applications such as anesthetics or anti-inflammatory ointments. 30 Murivenna oil, a medicated oil with A. vera, P. glabra, B. hispida, A. racemosus, and M. oleifera, known for their analgesic and anti-inflammatory properties, is applied externally for various ulcers, swellings, sprains, and fractures. The oil, with its soothing nature, helps alleviate pain and spasms, lubricating the anorectal area. Anal infiltration with Murivenna oil aids in reducing sphincter tone and associated symptoms. Triphalachoorna, acting as a laxative, also promotes wound healing, reduces discharge, and addresses diseases of tainted blood origin. The healing properties are attributed to the antimicrobial and debridement effects of tannic acid present in Triphala. 31, 32
Conclusion
This Systemic review can be concluded by the above mentioned finding that if symptom duration is less or in other words acute anal fissures conservative treatment methods can work very affectively especially with GTN. However as the duration of symptoms exceed the healing rate decreases attributing to the chronicity of the anal fissures thereby rendering the conservative treatment modalities less effective and making surgical treatment options like LIS the mainstay for chronic anal fissures.